When patients miss appointments, they interrupt the flow of patient care, impede clinic productivity, and signal an eroding patient loyalty. The rate of no-shows runs at 30% for the average family practice. A missed appointment amounts to missed billing revenue. Worse, if clinicians are part-time or full-time staff rather than contracted, they sit idle on the company clock, losing money with each passing minute. Finally, a missed appointment could be a symptom of a deserting patient, signaling a potential loss of long-term billing revenue.
Most clinics lose an average of 20% of their revenue due to missed appointments. Lost revenue may not be the largest problem caused by no-shows. Other problems span health damage, patient liability risks, reduced accessibility, and impeded resident education. Rigorous no-show management methods using advanced technologies integrate scheduling and billing data, reduce no-show rates, and improve associated revenues by more than 50%. They also mention the comparable improvement of long-term patient loyalty (Hashim et al., 2001).
No-Show Impact on the Clinic
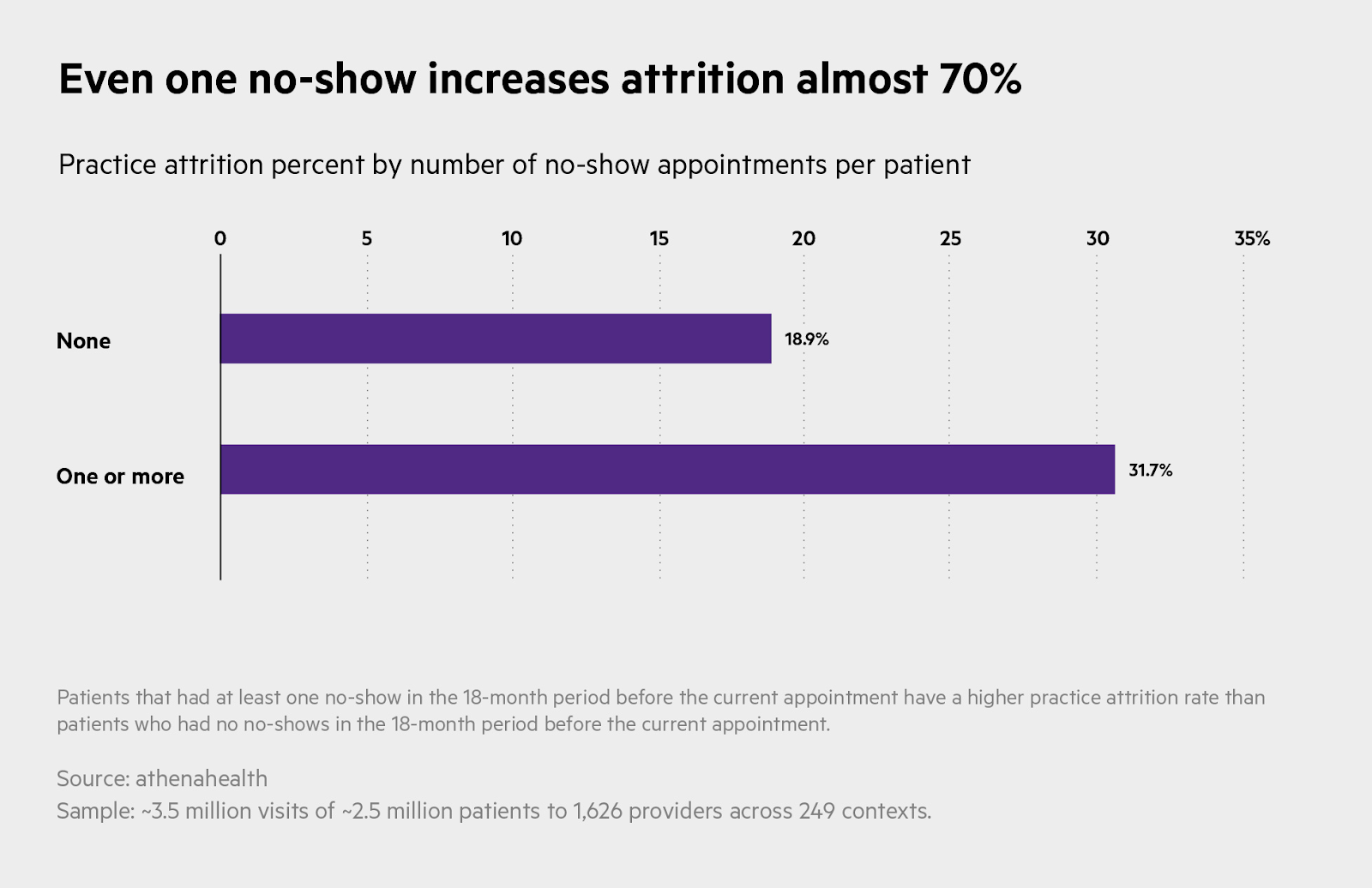
Figure 1. No-Show Impact (Hayhurst, AthenaHealth)
A missed appointment poses five kinds of problems:
- Health damage – A patient’s health can be damaged due to interrupted continuity of care or a missed opportunity to solve an acute health problem. The doctor also loses an opportunity for a timely review of patient health, treatment progress, etc.
- Liability risk – A patient who misses an appointment and suffers an injury may have a viable cause for a lawsuit against the practice. To avoid such risk, the doctor must maintain evidence of giving clear directions and making reasonable efforts to ensure the patient’s compliance with the care program, including keeping follow-up appointments.
- Reduced accessibility – Other patients are postponed and don’t get access to care because of a no-show or canceled appointment.
- Impedance to medical education – A resident or intern misses an opportunity to learn and improve care skills.
Loss of revenue – The clinic cannot make up revenue due to missed appointments. A financial impact arises from wasted resources, such as staff time, equipment, and facility utilization, that were allocated for the no-show patient.
No-Show Frequency Distribution
No-show rates average about 20%: 10% of clinics have less than 10% no-shows, 42% of clinics have 10%–20%, 34% of clinics have 20%–30%, and 14% of clinics have more than 30% no-shows (Izard, 2005). Further, the top 10 clinics regarding the lowest no-show rates range from 3%–9% for no-shows, while the bottom ten clinics reach 33%–57% (Moore et al. 2001).
Common reasons behind No-show
- Forgetfulness: Patients may simply forget about their appointments due to a busy schedule, lack of reminder systems, or cognitive factors.
- Transportation issues: Lack of transportation or difficulty accessing reliable transportation can prevent patients from attending appointments.
- Fear or anxiety: Some patients may experience fear or anxiety related to medical procedures, test results, or hospital settings, leading them to avoid or cancel their appointments.
- Financial constraints: Financial limitations, such as the inability to afford healthcare services or medications, may result in patients skipping or postponing appointments.
- Illness or emergencies: Patients may have unexpected illnesses or emergencies that prevent them from attending their scheduled appointments.
- Lack of awareness or understanding: Patients may not fully comprehend the importance of their appointments or the consequences of missing them, particularly for follow-up care or chronic conditions.
- Language and cultural barriers: Language barriers or cultural differences can impede effective communication and understanding, leading to missed appointments.
- Long waiting times: Lengthy wait times at hospitals can discourage patients from attending appointments, particularly if they have competing priorities or other time constraints.
- Stigma or fear of judgment: Patients with certain medical conditions or mental health issues may experience stigma or fear of judgment, causing them to avoid seeking care or attending appointments.
- Personal or work-related conflicts: Conflicts arising from personal commitments, work schedules, or other obligations may interfere with appointment attendance (Marbouh et al., 2020).
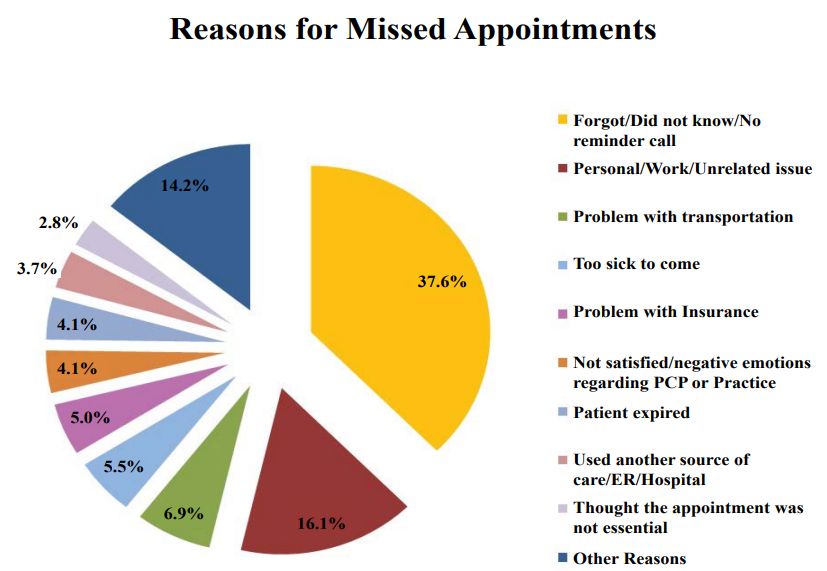
The image below shows common reasons for missed appointments (Saif et al., 2018).
According to a study, among all patients, those who never have a no-show appointment have an attrition rate of slightly less than 19 percent. In contrast, almost 32 percent of patients with one or more no-shows do not return to the same practice within 18 months (Hayhurst, AthenaHealth).
Three-Phase No-Show Management Strategy
An effective no-show management strategy is based on tracking, rescheduling, and follow-up:
- Tracking
- Record all no-shows and reconcile them with billing daily.
- Record no-show reasons and follow-up notes in patient records.
- Review end-of-day reports daily.
- Rescheduling in real-time
- Allow patients to request appointments online using the Internet
- Overbook and use waiting lists.
- Fill new openings with walk-ins or patients from the waiting list.
- Follow-up
- Activate a sequence of reminder calls/emails to all patients ten days, two days, and one day before their appointments.
- Place follow-up calls to determine reasons for no-shows and reschedule the patients. Reminder calls for upcoming appointments and follow-up calls on recent no-shows are effective strategies for billing revenue protection because they reduce the number of no-shows and help early identification of incipient patient attrition and other patient-related problems (Hashim et al., 2001).
- Follow up with warning letters after one no-show.
- Dismiss patients from the practice after three no-shows.
Reminder calls or emails before an appointment remains the most effective method to prevent missed appointments. Additionally, sending reminders via email and allowing patients to confirm online turns an office reminder into a patient’s action item, significantly outperforming the impact of a voice message or postcard. While recognizing the benefits of reminder calls, busy practice owners often neglect or postpone reminder and follow-up calls because of other office management priorities, such as personnel issues or billing. As with any other management initiative, a reminder call strategy must be implemented systematically and consistently to get results.
Note that outsourcing reminder calls to calling services and using the Internet reduce the cost of reminders. Therefore, reaching all patients before their appointments makes good business sense.
Ways to reduce No-shows
- Automation of appointment reminders: Implementing automated appointment reminders can significantly reduce no-show rates. Reminder call automation delivers the benefits of billing revenue protection and patient relationship management in a disciplined and systematic fashion and at a significantly lower cost. Using technologies, such as automated text messages or emails and third-party Tele-calling vendors, can save time and send reminders to patients before their scheduled appointments. Typically, a practice uses a new patient, an existing patient, a recall patient message, and several specialty messages. (Bano, 2022)
- Call Scheduling: The ability to schedule and automatically call patients with a personalized human voice message improves the efficacy of call scheduling and reduces no-shows
- Capturing feedback for issues or reasons behind cancellation: It is important to capture feedback from patients who cancel or no-show their appointments. This can be done through surveys or follow-up communication. Healthcare providers can identify recurring issues and proactively address them by understanding why cancellations or no-shows occur. It allows for improvements in scheduling and communication.
- Using communication methods preferred by patients: Patients may have preferred communication methods, such as text messages, emails, or phone calls. Healthcare providers should inquire about patients’ preferred communication channels during registration and use those channels to send appointment reminders or important updates.
- Using waitlist methods: Implementing a waitlist system can help fill available appointment slots due to last-minute cancellations. When a patient cancels, individuals on the waitlist can be notified and offered the opportunity to take the newly available appointment.
- Virtual appointments/telemedicine for patients with barriers such as transportation or time constraints: Virtual appointments allow patients to receive medical care remotely, eliminating the need for physical travel and providing greater flexibility. By providing alternative care options, healthcare providers can accommodate patients who might otherwise struggle to attend in-person appointments, reducing the likelihood of no-shows. (Huemor, 2023)
- High-quality infrastructure: A facility with the highest quality fiber optic feed and digital lines, allowing unsurpassed message quality and call progress detection accuracy. This technology helps to do the following:
- Avoid the pause accompanying most automated messages. In fact, any pause after the first sound could lead a patient to hang up or lead to an improper call diagnosis.
- Use call progress detection to determine if the phone was answered by a person or by an answering machine. This can mean the difference between leaving a complete message or only a short segment of the message on the answering machine.
When shopping for automated reminder services, focus on vendors that offer SaaS-driven service and pricing. “Software as a Service” vendors of reminder call automation solutions to price their services for only the calls they make, while you avoid purchasing hardware/ software and associated management and maintenance costs. In financial management terms, the SaaS proposition is equivalent to turning a capital expense into an operating expense, which translates into a better balance sheet and lower risk.
Three software features are especially useful in implementing the no-show management strategy outlined here:
1. End-of-day report– End-of-day reports display new patients, visits, cash, insurance, free visits, insurance billed and collected, cash collected, missed appointments, recalls, and average patient visits. An end-of-day report allows the manager to reconcile revenues with patient visits, eliminating no-charge visits and non billable appointments.
2. Scheduler– A scheduler can achieve the following:
- Allow patients access to an Internet-based appointment scheduler.
- Update the available appointment list due to cancellations.
- Alert about new openings for patients on the waiting list.
- Alert about appointments with missing authorizations.
Most schedulers allow monthly, weekly, and daily views. The “today” view should change colors for no-show appointments, prompting the front office person to follow up immediately or at the end of the day. A seamless method for retrieving appointment information without involving the medical staff. Ideally, the message scheduler should be integrated within electronic medical billing software, providing transparent access to both the patient appointment scheduler and the patient’s financial records.
3. Search feature– A search feature must allow you to find all no-shows within a specific time interval subject to specific patient names, attending physicians, CPT and/or ICD-9 code combinations, or other demographic conditions. Upon finding specific appointments, a “drill down” should be available to see the related appointment history or recurring appointment plan.
Using AI in No-Show Risk Management
- Intelligent appointment scheduling: AI algorithms can optimize appointment scheduling by considering various factors such as patient preferences, healthcare provider availability, and resource allocation.
- Appointment reminder optimization: AI can optimize appointment reminders’ timing, frequency, and content based on individual patient preferences and characteristics. AI algorithms can personalize and tailor appointment reminders to maximize their effectiveness by analyzing patient communication preferences, behavior patterns, and response rates. (Huemor, 2023)
- Risk stratification and targeted interventions: AI can assist in categorizing patients into different risk groups based on their likelihood of no-shows. Using predictive models, AI algorithms can identify patients at high risk of not attending appointments. Healthcare providers can then prioritize these patients for targeted interventions such as personalized reminders, additional support, or alternative care options to mitigate the risk of no-shows. (McCrary, 2022)
According to the AI-driven predictive model:
- Explores causes/factors: AI analyzes variables like age, gender, location, past records, and patient sentiments to identify factors influencing no-show rates.
- Learns from past data: Machine Learning trains the AI system using existing Electronic Health Records (EHR) data, enabling it to predict future no-shows more accurately.
- Mines data for patterns: AI algorithms analyze large datasets to uncover hidden relationships and trends contributing to no-show behavior, providing valuable insights for predicting appointment outcomes.
- Analyzes patient sentiments: AI can mine and analyze patient feedback from online/offline platforms, using Natural Language Processing (NLP) to predict no-show probability based on patient sentiments.
- Enables customization: The AI model can be customized to meet different clinics’ or organizations’ specific needs and objectives, enhancing its effectiveness in managing no-shows.
- Offers patient 360 views: By integrating data from various sources, AI provides a comprehensive patient profile, enabling personalized care, improved coordination, and informed decision-making. (Subramaniam, 2023)
Conclusion:
Missed appointments harm patient care, clinic productivity, and revenue. Clinics lose an average of 20% of their revenue due to no-shows, and the impact extends beyond financial losses, including health damage, liability risks, reduced accessibility, and impeded medical education. Implementing a comprehensive no-show management strategy, including tracking, real-time rescheduling, and effective follow-up methods, is crucial. Reminder calls or emails before appointments remain the most effective prevention method. Leveraging advanced technologies like AI can optimize appointment scheduling, personalize reminders, and identify high-risk patients.
Resources:
- Bano, R. (2022, September 15). 5 Proven Appointment Reminder Scripts to Reduce No Shows. Simple Texting. https://simpletexting.com/appointment-reminder-phone-call-script/
- Hashim, M. J., Franks, P., & Fiscella, K. (2001). Effectiveness of telephone reminders in improving rate of appointments kept at an outpatient clinic: A. ResearchGate. https://www.researchgate.net/publication/11982973_Effectiveness_of_telephone_reminders_in_improving_rate_of_appointments_kept_at_an_outpatient_clinic_A_randomized_controlled_trial
- Hayhurst, C. Even one missed appointment risks retention | athenahealth. Athenahealth. https://www.athenahealth.com/knowledge-hub/financial-performance/no-show-effect-even-one-missed-appointment-risks-retention
- Huemor. (2023, March 1). 8 Ways to Reduce Patient No-Show Rates | WELL Health. Artera. https://artera.io/blog/patient-no-show-rates/
- Izard, T. (2005). Managing the habitual no-show patient. ResearchGate. https://www.researchgate.net/publication/7956334_Managing_the_habitual_no-show_patient
- Marbouh, D., Khaleel, I. M., Shanqiti, K. A., Tamimi, M. A., Simsekler, M. C. E., Ellahham, S., Alibazoglu, D., & Alibazoglu, H. (2020). Evaluating the Impact of Patient No-Shows on Service Quality. Risk Management and Healthcare Policy, Volume 13, 509–517. https://doi.org/10.2147/rmhp.s232114
- McCrary, J. (2022). 10 Ways to Reduce Patient No-Shows. LeadSquared. https://www.leadsquared.com/industries/healthcare/reduce-patient-no-shows/
- Moore, C. G., Wilson-Witherspoon, P., & Probst, J. C. (2001). Time and money: effects of no-shows at a family practice residency clinic. Family medicine. https://pubmed.ncbi.nlm.nih.gov/11456244/
- Saif, U., Sangeetha, R., Todd, L., Ellen, D., Regina, J., Swapna, A., Christina, G., & Angad, G. (2018). Why do Patients Miss their Appointments at Primary Care Clinics? (Vol. 4). https://doi.org/10.23937/2469-5793/1510090
- Subramaniam, A. (2023, May 18). AI-Powered Patient No-Show Prediction for Improved Healthcare Business. KANINI. https://kanini.com/blog/ai-powered-patient-no-show-prediction-for-improved-healthcare-business/
A Future Book Publication Note:
This article is a chapter in the forthcoming 2nd Edition book “Medical Billing Networks and Processes,” authored by Dr. Yuval Lirov and planned for publication in 2024. We will post more chapters on this blog soon.


