How to Capture Images (Photos, Images), via the MyClinicMind Mobile App and Place Directly Into The Patient Chart
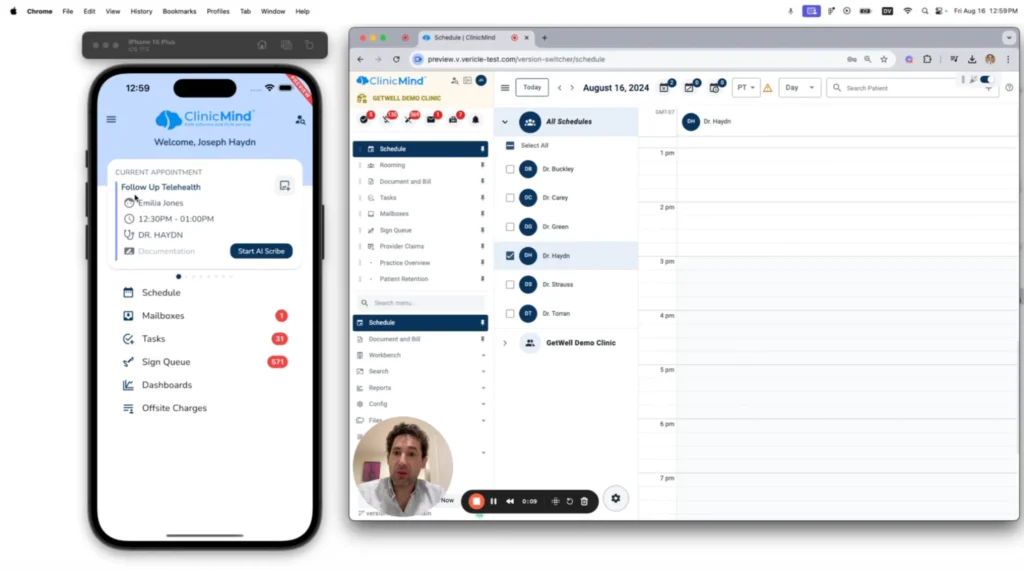
In this video, Dr. Roy Lirov demonstrates how to capture images using the UM ClinicMind mobile provider app. He walks through the process of adding images to a patient’s record, showcasing how easy it is to document visual information. Watch and learn how seamless it is to save and access images for patient records.
Celebrating Chiropractic Excellence
Welcome to Genesis Nation! Today, We are thrilled to introduce Dr. Justin Ohm from the International Chiropractic Pediatric Association (ICPA). With a rich history in chiropractic care, Dr. Ohm has been instrumental in shaping the future of the ICPA. In this blog post, we will delve into Dr. Ohm’s personal journey as a second-generation chiropractor, his mother’s significant contributions to the ICPA, and the broader vision that has guided their work in pediatric chiropractic care. A Legacy of Chiropractic Care: Dr. Justin Ohm’s Personal History Dr. Justin Ohm grew up in a home where chiropractic care was a way of life. His parents operated a home office, and from a young age, he was immersed in the world of chiropractic care. This early exposure laid the foundation for his deep understanding and passion for the profession. “I kind of grew up with it,” Dr. Ohm recalls. “My parents had a home office, so I really kind of grew up with it. When we were making too much noise back in the house portion of the house, my mom would say, ‘What are you doing?’ if she was with a new patient.” This environment not only instilled in him a sense of discipline but also a profound appreciation for the impact chiropractic care can have on individuals and families. The Formation and Growth of the ICPA The ICPA was founded in 1986 by Dr. Larry Webster, a visionary in the field. The association was established in response to a law in Connecticut aimed at limiting access to chiropractic care for patients under the age of 12. Dr. Webster recognized the need for a certification to validate pediatric chiropractic care, leading to the creation of the ICPA and its postgraduate education program. Tragically, Dr. Webster passed away in the late 1990s. During this challenging period, his wife Connie and the board of directors stepped in to provide direction and stability. It was around this time that Dr. Ohm’s mother took on the role of director, significantly contributing to the association’s growth. From 500 to Over 6,000 Members: A Testament to Leadership Dr. Ohm’s mother played a pivotal role in expanding the ICPA. Under her leadership, the association grew from approximately 500 members to over 6,000 members in about 15-20 years. This remarkable growth is a testament to her dedication and vision for the organization. “The ICPA literally kind of moved to my house,” Dr. Ohm shares. “The house that I was growing up in. So, the ICPA was very much a part of our lives growing up.” Her efforts not only increased membership but also enhanced the association’s reputation and influence within the chiropractic community. Transitioning Leadership and Embracing Challenges Following the passing of his mother in 2019, Dr. Ohm stepped into the role of director. Familiar with the staff, board, and instructors, he was well-equipped to lead the organization through a transitional period. However, the onset of COVID-19 presented unforeseen challenges, disrupting the traditional business model of in-person seminars. Fortunately, Dr. Ohm’s mother had the foresight to begin recording ICPA courses professionally a year before her passing. This initiative allowed the association to pivot to online learning, ensuring continuity in education and training despite the pandemic. The Unique Culture of the ICPA: An Extended Family Dr. Ohm attributes the unique culture of the ICPA to its foundation as an extended family. His mother’s approach was fiercely protective of the members, fostering a supportive and nurturing environment. This ethos has permeated the organization, creating a community of passionate and motivated chiropractors dedicated to family wellness. “The ICPA is kind of really an extended family, so to speak,” Dr. Ohm explains. “My mom was kind of like a mom to a lot of people in that sense. She was fiercely protective of her members.” This sense of community is evident in the joyful and compassionate atmosphere at ICPA seminars and events, setting it apart from other professional gatherings. The Impact of Webster Certification and Holistic Family Care One of the most well-known contributions of the ICPA is the Webster Certification, a technique that has gained recognition both within and outside the chiropractic profession. Dr. Ohm’s mother personally trained over 10,000 chiropractors in this technique, emphasizing its importance for perinatal care. “Webster certification is really becoming well known, ubiquitous almost, outside of the profession,” Dr. Ohm notes. “She trained over 10,000 chiropractors in that technique.” This technique supports balance throughout pregnancy, promoting a safer and more gentle birth process. The impact of this care extends to the newborn, fostering a healthier start to life. A Vision for the Future: Salutogenic Chiropractic The ICPA’s approach is rooted in a salutogenic mindset, focusing on enhancing health and adaptability rather than treating diseases. This perspective aligns with broader wellness trends, such as the biohacking movement, which seeks to optimize the body’s natural functions. “Salutogenic Chiropractic has such a place in that future,” Dr. Ohm emphasizes. “It’s about how do we add health, how do we add adaptability.” This approach not only resonates with practitioners but also appeals to families seeking holistic care for their children. Certification Programs and Professional Development The ICPA offers a range of certification programs to support chiropractors in providing specialized care. These include: Webster Certification: A foundational course for perinatal care. Perinatal Certification: An 80-hour program encompassing various aspects of pregnancy care. Pediatric Certification: A comprehensive 200-hour program focusing on care for children. Diplomate Program: An advanced certification requiring publication and extensive training. These programs equip chiropractors with the knowledge and skills to deliver high-quality care and support family wellness. Key Takeaways Leadership and Vision: Dr. Ohm’s mother’s leadership was instrumental in growing the ICPA from 500 to over 6,000 members. Resilience and Adaptability: The ICPA successfully transitioned to online learning during the COVID-19 pandemic, thanks to foresight and innovation. Community and Culture: The ICPA fosters a supportive, family-like environment, emphasizing compassion and holistic care. Salutogenic Approach: The ICPA’s focus on enhancing health and adaptability aligns with contemporary wellness trends. Comprehensive Certification
Mastering the Documentation Jungle
Welcome to the latest episode of Genesis Nation, where industry experts converge to unravel the intricacies of chiropractic practice and technology. In this captivating discussion, Dr. Gregg Friedman takes center stage, shedding light on the often underestimated yet pivotal aspect of documentation in chiropractic care. Unveiling Bulletproof EMR: The Convergence of Practice and Technology Dr. Friedman, a distinguished chiropractor with over three decades of experience, unveils the genesis of Bulletproof EMR. Drawing from his unique perspective as both a practitioner and innovator, he shares the inspiration behind crafting a documentation system that not only streamlines workflows but also ensures adherence to stringent regulatory standards. Reflecting on his journey from the era of floppy disks to the dawn of cutting-edge solutions, Dr. Friedman reminisces about the evolution of documentation software. From the cumbersome days of Scantron forms to the advent of palm-sized devices, he highlights the transformative power of technological innovation in revolutionizing chiropractic practice. The Catalyst: A Pivotal Personal Injury Case A pivotal moment in Dr. Friedman’s career came with a personal injury case that sparked a revelation regarding the critical importance of comprehensive documentation. Faced with the demand for meticulous records from insurance companies, he embarked on a three-year quest to unravel the elusive standards governing chiropractic documentation. Decoding CMS Guidelines: The Key to Compliance Dr. Friedman’s immersion into the world of independent medical examinations unearthed glaring deficiencies in chiropractic documentation practices. Central to his revelation was the recognition of CMS guidelines as the gold standard for demonstrating treatment efficacy. By aligning documentation practices with specific metrics mandated by CMS, chiropractors can not only enhance patient care but also safeguard their practices against audits. The Blueprint for Effective Documentation Drawing from his vast expertise, Dr. Friedman distills the essentials of effective documentation: Precision in Assessment: The assessment section of the SOAP note emerges as a linchpin for showcasing treatment outcomes. By meticulously documenting improvements in pain intensity and frequency for each condition, chiropractors can provide irrefutable evidence of treatment efficacy. Functional Outcome Questionnaires: Transitioning from generic pain scales to targeted functional questionnaires empowers chiropractors to gauge patient progress accurately. Simplifying questionnaire formats ensures patient compliance and yields actionable insights for tailored care plans. Trial-Based Care Planning: Embracing a trial-by-trial approach enables chiropractors to adapt dynamically based on patient response. Documenting measurable improvements at the end of each trial not only justifies ongoing care but also fosters patient engagement and satisfaction. Empowering Practitioners: A Call to Action In conclusion, Dr. Friedman dispels the myth of documentation intimidation, urging chiropractors to embrace a proactive stance towards compliance. With Bulletproof EMR as their ally, practitioners can navigate the documentation landscape with confidence, ensuring optimal patient outcomes and practice success. Join the Conversation For those eager to delve deeper into the nuances of chiropractic documentation and compliance, Dr. Friedman’s webinars and speaking engagements offer invaluable insights and continuing education credits. Stay tuned to Genesis Nation for updates on upcoming events and empower yourself to thrive in the ever-evolving world of chiropractic care. In the pursuit of excellence, let us heed Dr. Friedman’s guidance and embark on a journey of mastery in chiropractic documentation. Together, we can elevate our profession and transform lives, one meticulously documented SOAP note at a time.
Discovering Resilience and Vision
Welcome back, Genesis Nation! Today, we have a truly inspiring guest with us—Dr. Courtney Gowin. Not only is she a chiropractor, but she’s also an author, entrepreneur, and devoted mother of three. Her journey is a testament to resilience, vision, and the power of manifestation. Let’s dive into her story and explore the remarkable path she’s taken to create a life filled with purpose, abundance, and unwavering commitment to maternal health and pediatrics. The Genesis of Dr. Gowin’s Vision Dr. Gowin’s journey began in an unconventional way. She grew up as a fourth-generation cattle farmer, learning the value of hard work and grit from a young age. “Being able to just make things happen out of nothing,” she recalls, was a skill she honed on the ranch. This tenacity would later become a cornerstone of her success. Entering chiropractic school with a 13-page business plan, Dr. Gowin was determined to make her mark. Despite early setbacks—like her professor pointing out a spelling error in her plan—she remained undeterred. Her vision was clear: to collaborate with like-minded professionals and focus on maternal and pediatric health. Manifesting a Dream Practice Dr. Gowin’s journey to establishing her practice is nothing short of serendipitous. With a clear vision in mind, she manifested a Victorian home with a red mailbox and flowers out front—her ideal practice location. Scrolling through Craigslist one day, she found exactly that. Despite financial challenges, she negotiated her way into the building, starting her practice on a shoestring budget. “I went to dumpsters and picked up furniture, refinished it, refurbished it,” she shares. This determination paid off, and ten years later, her practice is thriving. Overcoming Personal Struggles Two years into her practice, Dr. Gowin faced severe postpartum depression. During this challenging time, she was presented with an opportunity to expand her practice into a full maternal wellness center. Despite the immense pressure and financial strain, she trusted her vision and took the leap. Today, her wellness center offers a comprehensive range of services, including pelvic floor therapy, pediatric therapy, massage, acupuncture, and more—all centered around maternal health. The Power of Grit and Vision Dr. Gowin emphasizes the importance of grit, especially during the hardest times. “Grit comes in whenever you feel like you’re failing, whenever you really feel like giving up,” she explains. However, she acknowledges that grit alone is not sustainable. It’s when grit is connected to vision and purpose that “the magic happens.” Having a clear vision acts as a guiding star, pulling you through the toughest times. Wanderlearn: A Manifestation of Passion and Purpose One of Dr. Gowin’s most exciting ventures is Wanderlearn, a company born from her personal journey of healing and self-discovery. After her divorce, she began taking herself on mini-retreats to heal. These experiences inspired her to create retreats for others, combining wellness, adventure, and continued education. Wanderlearn offers unique retreats like surf trips in Costa Rica, yacht excursions in Greece, and hiking in Switzerland. These retreats are designed to provide chiropractors with a space to heal, rejuvenate, and earn continuing education credits. “If you build a business around community and experience, it’s very sustainable,” Dr. Gowin believes. The Be-Do-Have Philosophy Central to Dr. Gowin’s success is the Be-Do-Have philosophy. She emphasizes the importance of being clear about who you want to be, what you need to do, and what you want to have. This mindset shift allows you to reverse-engineer your goals, ensuring that your actions are aligned with your vision. Practical Tips for Unleashing Your Creative Potential For those feeling stuck or overwhelmed, Dr. Gowin offers practical advice: Disrupt Your Rhythms: Take yourself out of your day-to-day environment. Travel, if possible, or create a dedicated space in your home for creativity and reflection. Engage in Physical Activity: Movement can stimulate creativity. Running, yoga, or any form of exercise can help clear your mind and spark new ideas. Consistent Reflection: Make time regularly to sit quietly, reflect, and write. Even if it’s difficult at first, this practice can lead to profound insights and breakthroughs. Final Words of Wisdom Dr. Gowin’s journey is a powerful reminder that we all have the capacity to create the life we envision. “You have one life and one fingerprint to leave on this world,” she says. “Make it count.” Her story of resilience, vision, and manifestation serves as an inspiration to us all. For more information on Dr. Gowin’s practice and Wanderlearn retreats, be sure to check out the links below. And remember, Genesis Nation, live well, love hard, and keep pursuing your dreams with unwavering determination.

