PatientHub Recognized by G2 for Patient Engagement
PatientHub Recognized by G2 for Patient Engagement When you run a clinic, you don’t measure success by clicks, badges, or even revenue alone. You measure it by the people who keep walking through your door. The mom who finally feels heard. The patient who shows up for every appointment because you made it easy. The person who, after months away, decides to come back because you reached out at just the right time. That’s what patient engagement really is: keeping people connected, engaged, and loyal—because healing happens through relationships. Recently, ClinicMind was recognized by G2 for Patient Engagement. For us, it wasn’t about the award itself—it was about what it meant. Providers are telling the world: this works. Patients are staying connected. Practices are growing, not just through billing, but through trust. At the center of that recognition is PatientHub. The Patient Engagement Challenges Clinics Face The phone rings while your staff is already juggling three patients. A no-show leaves an empty slot and lost revenue. A first-time patient falls through the cracks because no one had time to follow up. After hours, every missed call feels like another missed opportunity. These aren’t small inconveniences—they’re the moments that decide whether a patient stays with you or slips away. How PatientHub Improves Patient Engagement PatientHub was built for this world—the one you live in every day. Here’s how it helps you not just survive, but thrive: 24/7 Patient Communication with Voice AI & Chat: With Voice AI and our 24/7 Chat Bot, every patient gets an answer—even if it’s midnight. Bookings happen instantly. FAQs get handled automatically. No more missed opportunities, no more apologies. Reduce Patient No-Shows with Automated Reminders: Automated reminders by text, email, or voicemail cut no-shows by up to 38%. That means steadier schedules, steadier revenue, and fewer gaps in patient care. Centralized Patient Communication Hub: Instead of chasing emails, voicemails, and texts across different systems, PatientHub gives you a central engagement hub. Every message, every history, every patient—all right where you need it. Patient Reactivation & Nurture Campaigns: Our Reactivation and Nurture Campaigns quietly work in the background, reaching out to patients who haven’t been in for a while and keeping active patients engaged between visits. You focus on care—we handle the follow-up. AI-Powered Patient Reviews & Reputation Management: With AI-powered review responses and automated review boosters, PatientHub makes sure every patient feels heard, while also building the reputation that attracts the next new patient. Why Patient Engagement Tools Matter Today Patients today expect more than appointments—they expect connection. They want to know you’re listening, that you’re available, and that their care doesn’t end when they leave the office. For chiropractors and clinicians, this isn’t about “keeping up with technology.” It’s about staying human in a world that’s moving faster every day. PatientHub doesn’t replace relationships—it protects them. The Real Story Behind the Recognition The G2 recognition wasn’t about us. It was about you—the providers who use PatientHub to turn missed calls into new bookings, empty chairs into filled appointments, and one-time visits into lifelong relationships. Because when patients feel connected, they stay. They heal. They trust. And that’s what PatientHub is really about. Want to see how PatientHub can strengthen your patient relationships? Book a demo and experience what true engagement feels like. Book a free consultation
Credentialing Readiness Assessment Checklist for Healthcare Practices
Use this checklist to see how prepared your practice is for a successful credentialing process. Readiness matters because delays can lead to lost revenue, denials and compliance issues. The more items you check, the smoother your credentialing journey will be. 📁 1. Organizational Information for Credentialing ☐ Legal business name matches IRS records ☐ Tax ID Number (TIN) and NPI are active and valid ☐ Business entity is properly registered (LLC, PC, etc.) ☐ Up-to-date malpractice insurance with correct policy details 👤 2. Provider Documentation Needed for Credentialing ☐ Valid professional license(s) in all practicing states ☐ Board certifications and continuing education records ☐ DEA certificate (if prescribing medications) ☐ State-controlled substance registration (if applicable) ☐ Up-to-date CV (chronological, no unexplained gaps) 📋 3. Practice Operations ☐ Office address and phone number are current ☐ W-9 form is completed and signed ☐ Business hours and services offered clearly documented ☐ Staff roles and titles are defined 💻 4. CAQH, NPPES & Online Credentialing Profiles ☐ CAQH profile is completed and attested ☐ All documents uploaded to CAQH are current ☐ NPPES profile is accurate (NPI registry) ☐ PECOS enrollment is active (for Medicare providers) 💰 5. Insurance Payer-Specific Credentialing Readiness ☐ Target list of insurance payers is created ☐ Knowledge of each payer’s requirements and timelines ☐ Ready to submit applications individually or via delegated credentialing 📦 6. Internal Credentialing Process ☐ Dedicated staff or team for credentialing ☐ Timeline expectations set (90–150 days on average) ☐ Process in place to follow up with payers regularly ☐ Method to track application statuses 📉 7. Risk Factors That Delay Credentialing ☐ No past license suspensions or malpractice issues ☐ Gaps in work history are clearly explained ☐ No disciplinary actions by state boards 🧭 Scoring Your Credentialing Readiness ✅ 24–28 checks: Credentialing-Ready – You’re in great shape to start or streamline your credentialing. ⚠️ 15–23 checks: Partial Readiness – You’re close, but gaps may slow you down or lead to denials. ❌ 0–14 checks: At-Risk – Credentialing delays, rejections, or payer issues are likely without support. 👉 Not Fully Ready? We’ve Got You. CredEdge handles credentialing from start to finish. Document collection, application submission, payer follow-ups, and compliance monitoring. 🎯 Get Expert Help with Credentialing
Why ClinicMind Wins G2 Fall 2025 Awards for EHR, Billing & Patient Engagement
When you’re running an independent practice, software badges probably aren’t top of mind. What matters is whether your team can keep up with documentation, whether your reimbursements arrive on time, and whether your patients stay committed. That’s the real story behind ClinicMind’s G2 Fall 2025 recognition. Yes, we earned nine new awards across 20 categories, extending our leadership streak to 13 straight quarters and 35 total badges this year. But the badges aren’t the point. They’re simply proof of what happens when providers replace disconnected “Frankenstacks” with one unified growth platform. From Disconnected Tools to a Unified EHR & Billing Platform Too many practices still rely on pieced-together systems: one for billing, another for notes, a third for patient reminders, plus a maze of spreadsheets. Each gap creates additional administrative work, increased payer delays, and more opportunities for revenue to be lost. ClinicMind was built to end that cycle. By bringing credentialing, billing, documentation, and patient engagement into a single compounding suite, we help providers: Recover revenue with faster, cleaner claims. Shrink admin time so staff can focus on patients. Boost retention with built-in engagement tools that keep patients connected. ClinicMind G2 Fall 2025 Awards: Real Recognition That Matters G2 users confirmed what our clients tell us every day: Momentum in billing and EHR shows practices are actively switching to unlock lost revenue. Leadership in chiropractic means providers can finally document faster and stay compliant without drowning in paperwork. High performance in small-business billing & EHR proves even lean teams can run like big ones. Recognition in patient engagement signals that growth isn’t just billing, it’s stronger patient relationships. And perhaps the most meaningful validation? The “Users Love Us” badge. That one can’t be bought; it comes directly from providers who’ve experienced the shift firsthand. What G2 Recognition Means for Your Practice Awards are nice, but no one buys software for a badge. The real win is when: Your staff feels less burned out. Your reimbursements arrive predictably. Your patients keep coming back. That’s what ClinicMind delivers and why recognition keeps compounding. See Why Practices Switch to ClinicMind Book your free consultation today and discover how one platform can replace your Frankenstack and protect your revenue. Read the full details in our official G2 Fall 2025 press release
How ClinicMind’s RCM Software + Service Reduced A/R Over 120 to 4%
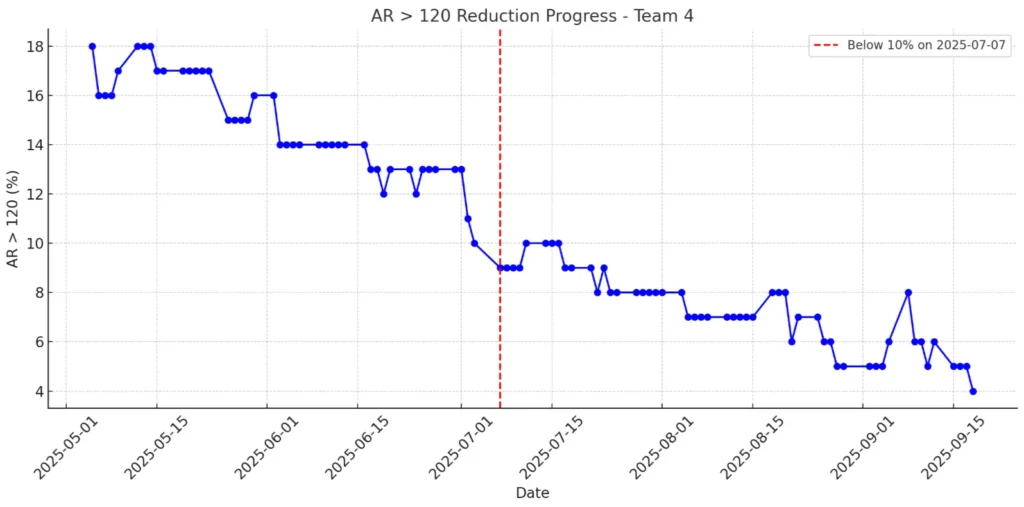
How ClinicMind’s RCM Software + Service Reduced A/R Over 120 to 4% In healthcare revenue cycle management (RCM), results are what count. Achieving numbers like these is rare. ClinicMind’s RCM Team recently reached an A/R over 120 days of just 4%, which is only a third of the industry average of 13.4% according to MGMA. This milestone didn’t happen by chance. It came from ClinicMind’s approach of blending strong RCM software with skilled human support. This system helps practices lower their aged A/R and speed up cash flow. What is A/R > 120, and Why Does It Matter? Accounts Receivable (A/R) aged beyond 120 days represents money practices may never collect. The higher the percentage, the greater the financial strain. With the industry benchmark sitting at 13.4%, many practices face delayed or lost revenue. ClinicMind’s Team kept their rate at just 4%, showing that practices can reach and maintain top results when they have the right tools and expertise. From 13% to 4%: ClinicMind’s 60-Day A/R Reduction Journey Late June 2025 Team was at 13%, aligned with MGMA benchmarks. In July 2025, our numbers improved steadily, moving from 12% to 9%, then 7%, and finally 6%. By August 2025, we held steady between 5% and 7%, finishing the month at 4%. Within 60 days, we cut our aged A/R in half and kept it at that level. ClinicMind RCM Software: Automating Revenue Cycle Management Our software helps you work more accurately, saves time with automation, and keeps everything clear. Daily RCM Dashboards: The 4% metric itself came from real time ClinicMind dashboards, providing transparency for clients and teams alike. Automated Denial Alerts: Same-day appeal workflows were triggered instantly by software, preventing delays. Bulk Patient Statements: Automated statement generation and small balance sweeps ensured no revenue was overlooked. Account Prioritization: Smart filters highlighted high-balance accounts, allowing teams to focus on the most critical accounts first. Expert RCM Services that Deliver Results Same-Day Appeals: Analysts acted immediately on flagged denials. Collector Focus: Experienced team members handled the top 20 high-balance accounts directly. Backlog Blitz: Analysts were temporarily reassigned to address the A/R over 120-day backlog. They worked at scale based on insights from the dashboards. The Result: Software created visibility and automation; the service team applied judgment, persistence, and expertise. This balance of technology and expert support is what makes ClinicMind a leader in healthcare revenue cycle management and RCM billing services. Why ClinicMind’s A/R Performance Matters for Practices Benchmark Beating: 4% vs. 13.4% shows ClinicMind delivers world-class outcomes. Consistency: This was not just a brief improvement. The ongoing performance trend shows that these results are sustainable. Scalability: The same playbook of software + service can be replicated across other teams and client BPOs. By combining RCM software with expert human support, ClinicMind helps practices achieve world-class revenue cycle optimization Software + Service = Sustainable RCM Success Technology by itself can’t fix revenue cycle challenges, and service alone won’t scale without the right data and automation. ClinicMind’s story shows that when smart software and expert service work together, the financial results are hard to beat. See how your practice can achieve industry-leading A/R results with the right technology and expert support – Book a consultation to learn more

