Update – August 19, 2024
Updates From Our CEO
Last February, we experienced the largest cyber attack in the nation’s history on our main clearinghouse – owned by the biggest payer. The cyber attack
- Disrupted claims submission and ERAs,
- Necessitated manual work, and
- Kicked us twenty-five years back into the late 90s.
Worse, according to an AMA report (https://www.ama-assn.org/press-center/press-releases/physicians-struggle-keep-practices-afloat-after-change-cyberattack), during this time, 55% of the small-to-medium practice owners needed to dip into their personal savings in order to cover practice expenses or make payroll.
Unitedhealth Group has also stated (https://www.unitedhealthgroup.com/newsroom/2024/2024-04-22-uhg-updates-on-change-healthcare-cyberattack.html) that due to the complex nature of the breach, it may take several months to identify and notify impacted individuals. “62% are still dipping into personal funds to cover practice expenses, 42% still can’t afford to buy supplies, and 34% can’t make payroll.”
But this story starts earlier, long before February: in October 2022, UnitedHealth Group closed its acquisition of Change Healthcare, the largest claims clearinghouse in the U.S. Why would one of the four largest insurance companies need to control a healthcare insurance claim gateway to all payers? What added value could be brought to the table except for an attempt to achieve control of the providers’ claim flow to other payers?
And so, while the entire world aims at IT democratization and applies Artificial Intelligence to accelerate the future prosperity through automation, one of our largest payers reversed the progress direction by trying to monopolize the providers’ access to payers and gave us a taste of how massively centralized solutions feel when things go wrong.
Followup Questions:
- Why wasn’t the cyber attack immediately solved?
- Who benefits from the delay?
These questions will be addressed in the future. In the meantime, we must do everything under our control to solve the problems caused by the cyber attack of one of the largest payers:
1. We have found alternative clearinghouses. This process requires enrolling the clients again and that depends on two kinds of teamwork
a. client cooperation – we cannot make progress until the client responds.
b. payer cooperation – why would they be in a rush? Especially when EVERYBODY is also re-enrolling at the same time.
c. We have completed three-quarters of the needed enrollments
d. Real time eligibility is back up and running for all payers, and patient statements are being turned back on today, unless we hear from you, as stated in our previous correspondence.
2. We maximized the use of ClinicMind’s automation at every stage by splitting the workload in two parts, addressing separately he claims that have already received the new ERAs because of the newly functioning automation and the claims that are inaccessible to the new ERAs. These claims require manual payment update and followup.
3. We have hired and trained more staff to do the necessary manual work. The replacement of automated processes with human resources required accelerated hiring and training at an unprecedented scale, with 40-50 new hires a month.
4. We have also hired a dozen of third-party RCM companies to increase our capacity. While many BPOs went out of business because of the cyberattack, we have found and trained an additional 14 new BPOs.
- Call Center at (234) 254-2255
- Open a ClinicMind task directly to your Coach or Admin
- Click Chat Now from at the top navbar on any page of the ClinicMind system
a. Click Chat with us
b. When asked what the Topic of the chat is, Select Billing Question
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring billing normality.
Update – July 15, 2024
Updates From Our CEO
Weekly Update:
We continue to see improvement and hope to return to normal operations by September.
We are about 24% complete with the ERA enrollment project, and we recently signed up fourteen RCM BPO teams to help us work through our work backlogs, which accumulated because of the Change HealthCare Clearinghouse cyberattack.
Please compare your practice insurance collections prediction on your ClinicMind Home screen and contact us with any questions using one of these three methods:
- Call Center at (234) 254-2255
- Open a ClinicMind task directly to your Coach or Admin
- Click Chat Now from at the top navbar on any page of the ClinicMind system
- Click Chat with us
- When asked what the Topic of the chat is, Select Billing Question
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring billing normality.
Update – July 5, 2024
Updates from our President, ClinicMind Professional Services Division
Weekly Update:
We have important news about the Change Healthcare outage and how it’s affecting your practice. Stay informed with the latest insights directly from Dr. Brian Capra, President of ClinicMind Professional Services Division.
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring normality.
Update – June 28, 2024
Updates From Our CEO
Weekly Update:
The Change Healthcare clearinghouse debacle has affected all insurance billing. It’s so bad that a fund has been created to help doctors.
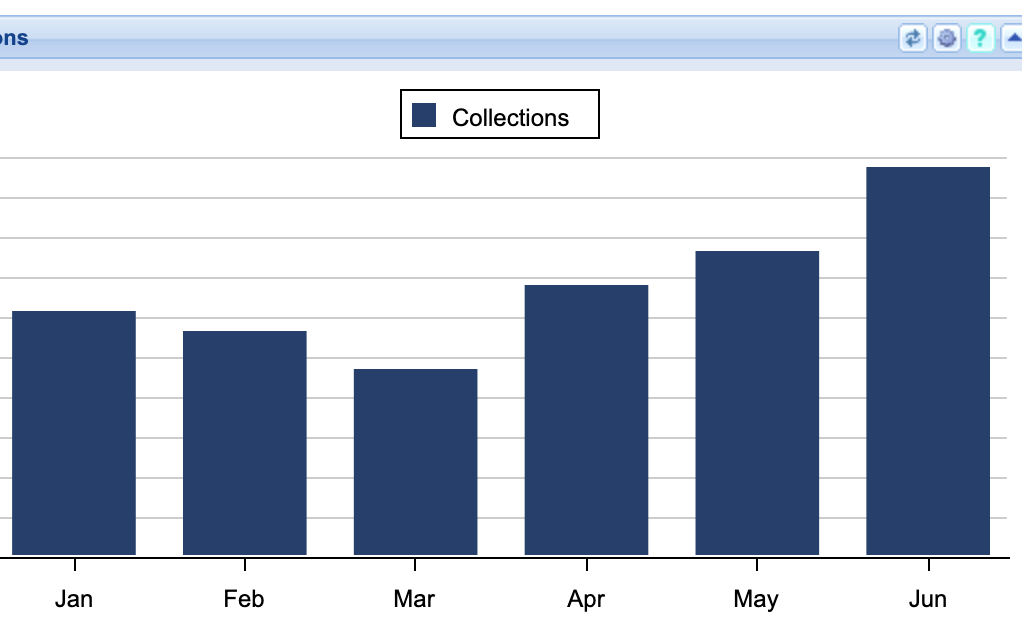
This chart, which is available on the Home page of the ClinicMind system, illustrates the following points:
- We are with you, and our plan is not only working, but it has EXCEEDED our efforts expectations:
- Our monthly collective collections have DOUBLED since March
- Compare this chart to the chart we posted on this Blog on June 6, where we made and posted an optimistic but more conservative prediction.
- Our Plan has five parts:
- We have separated our institutional (CMS-1500) and professional (UB-04) teams so that each team can focus on their unique problems
- Both teams have split their claims into two groups and allocated dedicated resources for:
- the current A/R to make sure the new money continues to flow in
- the old A/R accumulated before and during the outage
- Our HR Division continues to hire experienced resources to meet the growing demand for our services.
- Our Training department built an accelerated training course for the Change Health Clearinghouse Outage Management Training.
- Completing ERA enrollments remains a high priority: Many payers require a provider’s signature, and your prompt cooperation is encouraged and appreciated.
Please compare your practice insurance collections prediction on your ClinicMind Home screen and contact our Call Center at (234) 254-2255 or open a ClinicMind (Genesis) task to schedule an appointment with your Practice Coach or Admin to review any differences unique to your practice and any improvement steps we need to take above and beyond our current efforts.
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring normality.
Update – June 21, 2024
Updates From Our CEO
Weekly Update:
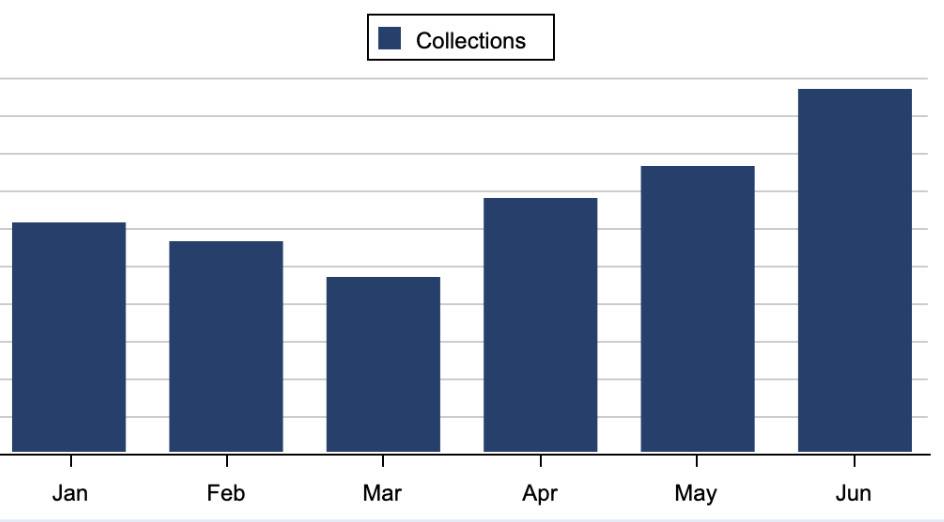
Our collections graph on our home page continues to look promising for June. Sadly, this is a result of extra manual work because of the continued impact of the Change Healthcare outage.
If your own graph does not look similarly promising, please contact us via email, create a ClinicMind (Genesis) task, or by phone at (234) 254-2255
We continue to work on ERAs and enrollments, and are making steady progress. See this attached image:
Update – June 6, 2024
Updates From Our CEO
Weekly Update:
ClinicMind predicts our Customer Insurance Collections will continue to climb in June, making up for the payment delays caused by the colossal Change Healthcare Outage in February and March.
The attached chart shows the average insurance collections bar chart shape across thousands of providers using the ClinicMind system. Its optimistic shape is due to the amazing teamwork between our clients, our software engineers, our Revenue Cycle Managers, and our AR follow-up analysts.
The ERA disruption caused by the Change Healthcare outage has not been corrected yet, which continues to cause major claim processing backlogs. Our RCM teams continue to find manual workarounds to compensate for the automation disruption, including re-enrollments and patient statement generation. There is still no ETA for the real-time eligibility test.
Please compare your practice insurance collections prediction on your ClinicMind Home screen and contact our Call Center at (234) 254-2255 or open a ClinicMind (Genesis) task to schedule an appointment with your Practice Coach or Admin to review any differences unique to your practice and any improvement steps we need to take above and beyond our current efforts.
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring normality.
Update – May 29, 2024
Updates From Our CEO
Weekly Update:
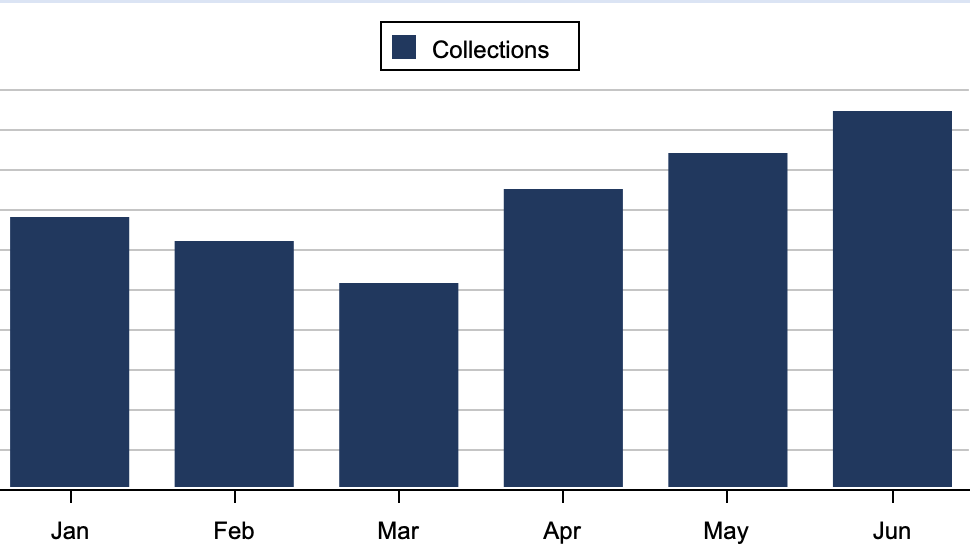
The effect of the outage is not over yet, but this illustration that is available on your ClinicMind Home Page shows that the worst is behind us:
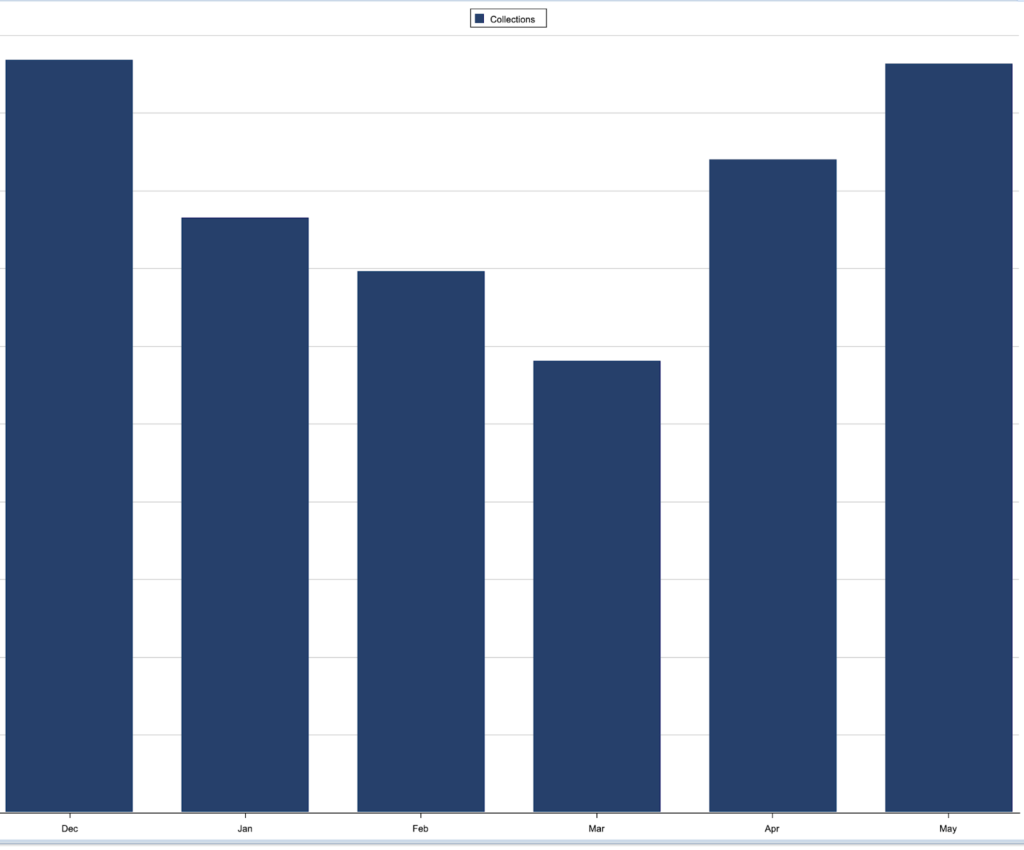
Dec Jan Feb Mar Apr May
This bar chart for monthly insurance collections shows the dip caused by the CHC outage in February and March and our partial and accelerating recovery in April and May.
I have complete confidence in our team and software to overcome this unprecedented outage. Thank you for your continued trust in ClinicMind
Update – May 23, 2024
Updates From Our CEO
Weekly Update:
- Our electronic claim submission is restored to its full pre-CHC outage capacity. All claims previously dropped to paper to bypass the Change Healthcare outage have since been submitted electronically as needed.
- We continue the process of re-establishing ERAs, which will likely take several weeks and could require your assistance in signing new enrollment forms.
- In the absence of these enrollment forms, we manually obtain claim information using phone and portal access when available.
- Other work in progress:
- electronic eligibility service,
- a pathway to send patient statements, and
- a preferred submission path for secondary payers where the payer does not accept electronic claim submission.
Your ability to submit claims and receive payments promptly remains our absolute priority.
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring normality.
Update – May 16, 2024
Updates From Our CEO
Great News!
We successfully submitted 27,600 claims on Friday. In addition, we have resubmitted all previously dropped to-paper claims electronically.
Your ability to submit claims and receive payments promptly remains our absolute priority. Accordingly, while we wait for the approvals, we continue to work on expanding the lists of states and payers.
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring normality.
Update – May 9, 2024
Updates From Our CEO
We have successfully submitted 20,000 claims via our new Optum route, including Medicare of AL, VA, WV, SC, GA, TN, NC, and Aetna.
Note that many of these submissions are still pending approval, particularly in states where direct submission is not yet authorized. Your ability to submit claims and receive payments promptly remains our absolute priority. Accordingly, while we wait for the approvals, we continue to work on expanding the lists of states and payers.
Thank you for your continued trust in ClinicMind. We look forward to resolving these issues completely and restoring normality.
Update – May 6, 2024
A message from our CEO
The massive cyber-takedown of CHANGE HEALTHCARE has continued to have far-reaching results. In March, collections were down approximately 40% because of the outage. Many offices are struggling to meet payroll, rent, and other overhead. Worse, patient statements have not been sent since February 21st, 2024.
From Becker’s Hospital Review, we learned that “UnitedHealth believes that the hacker group ALPHV, known as BlackCat, entered the Change Healthcare portal, which was not protected by multifactor authentication, around nine days before they were aware of any cyberattack activity and exfiltrated data. On February 21, the hackers deployed ransomware.”
In light of the problem’s complexity and unknown time of resolution by UnitedHealth, since February 21st, ClinicMind’s team has been putting in countless hours to work around this. While individual practice collection improvements vary, in April, we recorded an average 30% improvement over March.
Your ability to submit claims and receive payments on a timely basis is our top priority:
- We added the ability to send claims on paper for claims that lost their standard electronic submission path or require new enrollments for electronic submissions. Over the past two weeks, we have dropped 15,000 claims to paper.
- We are working daily on EDI enrollments to re-enable electronic submission via alternative pathways for those payers who require enrollments.
- We are submitting directly to payers whenever possible. We have established limited direct connections to Medicare and continue establishing new ones.
- Completing ERA enrollments. Many payers require a provider’s signature, and your prompt cooperation is encouraged and appreciated.
- Also, providers are advised to collect expected co-payments and deductibles upfront whenever possible since patient statements have not been sent since February 21st, 2024.
We understand your concerns and thank you for your continued patience and understanding as these issues will be completely resolved in the coming months.
Update – April 18, 2024
We want to update you on the current service interruptions related to our connections with Change Healthcare (CHC). We are actively monitoring the situation and have implemented several measures to mitigate the impact on your services.
The way in which we connect to CHC is still down. We are testing that connection every morning and will immediately start working with them on rollouts for our supported services.
In the interim, we are working on the following:
- Adding the ability to send claims on paper and are in the testing phase. This will allow us to submit claims that do not otherwise have an electronic submission path or that require enrollments for electronic submissions.
- We are continuing to work on getting EDI enrollments completed to re-enable electronic submission via alternative pathways for those payers that require enrollments.
- We are working on establishing additional pathways for claims submission, including submitting directly with certain payers.
- ERA enrollments have also been started. Where possible, these are being completed completely by our internal team, but many payers require a provider signature. These enrollments are needed to reroute ERA and allow us to get the adjudication information from the payers. There are over 5,000 enrollments to be completed.
We have made some progress on establishing direct connections but are still in the testing phase. Not all payers accept claims in the same way across the board from each clearinghouse. This creates complexity and physical time spent chasing every avenue.
To say we are working tirelessly is an understatement, and we appreciate your patience throughout this frustrating ordeal.
It is also important to mention that CHC ‘Products will go through a phased reconnection process, including launch, testing and scaled reconnection.’ We have reached out to our rep and have not gotten a response yet on when we will be reconnected to any of the items that CHC is stating they have back up.
Once again, we sincerely appreciate your patience as we work together to navigate these challenges and restore normal operations.
Update – March 29, 2024
We understand the challenges the Change Healthcare outage has brought, especially with delayed payments and confusing updates.
Here’s how we’re addressing these issues:
- Payment Delays: We’re working tirelessly to manage these delays. Remember, if our work doesn’t result in your payment, it’s free.
- Clear Communication: We’ll continue to provide regular, straightforward updates to cut through any confusion.
Solutions in Action:
- Manual Processing: We’re working on getting paper claims submitted.
- Automated Approaches: We’re working on securing EDI approvals for efficiency.
- Your Role: Please promptly sign and return any forms sent via task by our enrollment team for ERA processing.
We’re in this together, and our commitment to your success is unwavering.
Thank you for your patience and trust in ClinicMind.
Update – March 25, 2024
As you know, the current CHC outage is impacting our ability to send out paper patient statements, which currently remain on hold.
Given these challenges, we strongly encourage the transition to electronic statements (e-statements). The CHC outage did not affect e-statements, which are available for those using Fortis or Cash Practice as their credit card merchant.
To set up e-statements, please contact us to update your account if you have any questions about this process. Our team is ready to assist you in making this transition as seamless as possible.
Thank you for your continued cooperation and understanding during this difficult period
Update – March 20, 2024
Today’s update regarding our ongoing situation with Change Healthcare is as follows: There is still uncertainty about when Change Healthcare will resume accepting claims. In light of this, we continue to re-enroll practices through alternative clearinghouses. This is a crucial step in ensuring our operations continue smoothly during this period.
In addition to this, we are actively exploring additional submission paths. Our team is collaborating with our current partner vendors to identify alternative solutions in cases where our existing clearinghouses may not be viable options. Our primary focus remains on getting claims submitted efficiently and effectively.
Alongside these efforts, we also focus on redirecting practices? Electronic Remittance Advice (ERA). This is an important aspect of our overall strategy to maintain seamless financial operations.
Your patience and understanding as we navigate these challenges are greatly appreciated.
Update – March 14, 2024
Change Healthcare (CHC) recently provided updates on their services, necessitating some clarifications.
Regarding Electronic Payments (ERA), it was initially expected that CHC’s system would be back online by 3/15. However, this date specifically refers to CHC processing payments from insurance companies to practices and not to the resumption of ERA services.
In terms of Claims Submission, the initial hope was to resume submissions by the week of 3/18. According to the latest information from CHC, this process is now expected to take several more weeks. The delay is due to the ongoing transition of enrollments to Optum?s alternative clearinghouse, extending the timeline beyond initial estimates.
Accordingly, in response to these delays, we are actively pursuing the alternative payer strategy initiated at the beginning of last week. To date, we have submitted a significant number of claims and have diligently followed up on a majority of payments. This proactive approach is aimed at mitigating the impact of the current situation.
We will continue to provide updates as more information becomes available.
Update – March 11, 2024
Major Update on Claims Processing
We are happy to announce a few updates to the ongoing cyberattack at Change Healthcare and subsequent effects it has had on our abilities to process claims.
Change Healthcare predicts a potential resumption of claim processing by March 18, 2024. However, as full operational capacity isn’t guaranteed by this date, they are set to launch electronic payment functionality from March 15th. This development is crucial as we await the reconnection of ERA services.
In the meantime, our team is actively pulling remittance advice through payer portals. We’ve successfully updated all payers that don’t require additional enrollments, and we are now focusing on payers needing enrollment. This effort requires gathering contact information to initiate enrollment and ensuring providers promptly receive and return the required forms.
Your cooperation in promptly returning requested forms will greatly assist in expediting this process for your practice. This effort is key to maintaining our high service standards and minimizing disruptions.
Thank you for your continued trust in ClinicMind.
Update – March 7, 2024
We are pleased to share some positive developments as we navigate through the challenges posed by the Change Healthcare/Optum outage:
- Efficient Claim Resubmission: We’ve successfully transitioned all claims previously on hold (Temp_Hold) due to the outage. These claims are now in the Valid category and have been resubmitted wherever we’ve identified viable alternative routes.
- Expansive Payer Network Update: Our team has diligently updated the submission pathways for over 600 payers, ensuring that claims are processed through these new, effective channels.
- Ongoing Strategic Efforts: Our commitment to resolving this issue is unwavering. We are actively exploring and establishing alternative pathways for the remaining payers, ensuring a comprehensive and robust solution to this challenge.
- Significant Progress in Claim Submissions: Despite the unexpected outage, we’ve made remarkable progress in claim management. To date, we have successfully submitted 75% of the total insurance claims that were impacted by the outage.
We appreciate your patience and understanding as we continue to work tirelessly to mitigate the impact of this outage. Our team is dedicated to maintaining the highest standards of service and efficiency during this period. Stay tuned for further updates as we forge ahead.
Update – February 29, 2024
As we continue to navigate the ongoing system outage at Change Healthcare, we want to provide you with the latest updates and address some new questions that have arisen. We understand the challenges this situation presents and appreciate your continued patience and understanding.
Persisting Problems
- Change Healthcare, the largest healthcare clearinghouse in the country has been experiencing an outage since February 21, 2024. This is a nationwide issue, affecting not just our services but many others across the country.
- Claims, Electronic Remittance Advice (ERA), eligibility checks, and paper patient statements remain queued for submission as soon as Change Healthcare resolves the issue. We assure you that electronic statements are still being sent out without interruption.
- This outage is causing delays in payment postings and our ability to follow up on claims. We are preparing for a significant backlog of claims once the problem is resolved, but rest assured, our team is ready to handle this efficiently.
New Updates
- In response to this outage, we are actively exploring alternative solutions. We are attempting to reroute claims through different clearinghouses.
Frequently Asked Questions
Q: Why are some of my claims in ‘Temp Hold’?
A: Claims are placed in ‘Temp Hold’ as a proactive measure due to the ongoing outage at Change Healthcare. This status is applied to claims that we are currently unable to submit through the usual channels. The ‘Temp Hold’ allows us to effectively identify, manage, and prepare these claims for alternative submission methods as soon as they become available. It’s a temporary step to ensure that your claims are securely held and ready for processing, minimizing any further delays once the system issues are resolved. We are actively working to transition these claims back to their valid status within the next day or two.
Q: How are Eligibility Services affected by the Change Healthcare outage?
A: Electronic eligibility services, which are provided by Change Healthcare, are included in the disruption caused by their system outage. This means that there may be delays or temporary unavailability in verifying patient eligibility through their system. We are monitoring the situation and will provide updates as they become available.
Q: Why am I seeing payments in my bank account that are not reflected in the system?
A: The payments you are seeing in your bank account are for claims that have already been processed and paid out by the payers. These transactions are continuing as usual. However, due to the ongoing outage at Change Healthcare, there is a disruption in the transmission of Electronic Remittance Advice (ERAs). Our system relies on these ERAs to post payments and generate accurate invoices. Without the ERAs, there is a temporary disconnect between the payments received in your bank account and what is currently reflected. We are aware of this issue and are working to resolve it as soon as the ERAs are back online. In the meantime, please be assured that your payments are secure, and we will update the system accordingly once the ERAs are received.
Invoicing
You might notice payments in your bank account that are not reflected due to the ERAs not being sent. This discrepancy is because payments for claims already received by payers are still being processed.
Consequently, your invoice this month might be lower than expected, with subsequent invoices potentially being higher as we catch up with payment postings, eventually achieving balance. If you encounter any issues reconciling your accounts, please reach out to our team for assistance.
Looking Ahead
The longer this disruption continues, the greater the backlog in the queue for submission and potential rejections once service is restored. We are committed to keeping you informed and minimizing the impact on your business.
We sincerely apologize for any inconvenience caused and are working tirelessly to find solutions and keep your operations running as smoothly as possible during this challenging time. For any further queries or concerns, please feel free to contact us.
Thank you for your continued trust in our services.
Update – February 25, 2024
We are writing to inform you of a significant ongoing situation that may impact our services to you. Change Healthcare, the largest healthcare clearinghouse in the country is currently experiencing a system outage that began on February 21, 2024. This is a nationwide event affecting users across the country.
Due to this outage, there are certain temporary disruptions in our usual processes. Specifically, the submission of claims, Electronic Remittance Advice (ERA), eligibility checks, and paper patient statements are currently on hold. These items are queued and will be submitted as soon as Change Healthcare resolves the issue. Please note that electronic statements are still being sent out without interruption.
This situation is leading to delays in payment postings and our ability to follow up on claims. We understand this may cause some inconvenience, and we are committed to addressing these challenges as efficiently as possible.
Change Healthcare is actively working to resolve this issue and is providing regular updates. We are closely monitoring the situation and will inform you as soon as we have more information. Unfortunately, there is currently no estimated time for when the system will be fully operational again.
For the latest status updates, please visit Change Healthcare Status Page.
Once the problem is resolved, we anticipate a significant backlog of claims. We want to assure you that our team is prepared and will diligently work to process all pending items as quickly as possible.
We ask for your patience and understanding during this time. The best course of action currently is to ‘sit tight’. However, we are here to address any concerns you may have. If you have specific questions or issues, please do not hesitate to open a task with us, and we will respond as promptly as we can.
We understand the critical nature of these services to your operations and are committed to keeping you informed and minimizing the impact on your business. Thank you for your patience and understanding as we navigate this challenge together.